Chemotherapy
Introduction
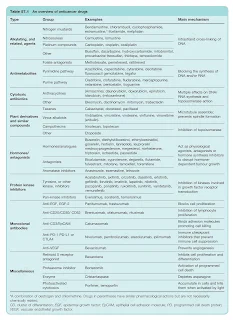
Cytotoxic drugs, along with surgery and radiotherapy, remain the mainstay of cancer treatment.
However, newer treatments based on targeting the specific malfunctions of cell cycle control that characterise cancer cells, and on increasing their susceptibility to immunological attack, are becoming increasingly important.
- These include hormone antagonists, kinase inhibitors and monoclonal antibodies.
Ministry of Health Systemic Therapy Protocol 2016
Ministry of Health Systemic Therapy Protocol focuses on chemotherapy and targeted therapies used in the treatment of solid tumours. Although it is not meant to replace international protocols, it is very useful in the local setting as a quick reference.
To all provisional registered pharmacists, I personally recommend you start the book from the chapter 14 and 15, specifically on these topics:
- Pre-Chemotherapy Assessment
- Important Formulas
- Management of Emesis
- Pre-Medication for Specific Chemotherapy
- Dose Modification Guidelines
- Febrile Neutropenia
- Chemotherapy Toxicities and Management Guidelines
- Safe Handling and Administration of Cytotoxics
- Extravasation
- Cytotoxic Spill Management
- Chemotherapy Preparation and Reconstitution
Only then, you may read up cancer and chemotherapy protocols relevant to your hospital setting.
On page 77, a minor typo error on EP-EMA regimen is suspected. The actinomycin D (dactinomycin) dose should be 0.5 mg per cycle as an absolute dose.
Chemotherapy Regimen
When you first enter cytotoxic drug reconstitution (CDR) department, you may have zero knowledge and feels like chemotherapy regimen is some alien language. However, in reality, chemotherapy regimen is not very different from how we manage a hypertension or diabetes mellitus.
In essence, chemotherapy regimen is like a protocol that we used specifically to treat a specific cancer. Often, multidrug chemotherapy regimens are clinically utilized and these regimens are typically referred to by their acronyms. To illustrate,
- Breast Cancer - FEC, FAC, Docetaxel
- Colorectal Cancer - De-grammont, Mayo, FOLFOX, FOLFIRI, XELOX
- Gestational Trophoblastic Disease - EMA-CO
- Hodgkin Lymphoma - BEACOPP, ABVD
- Multiple Myeloma - VCD
- Non-Hodgkin Lymphoma - R-CHOP
- Ovarian Cancer- Carboplatin/Paclitaxel, Cisplatin/Paclitaxel
However, traditional chemotherapy lacks selectivity, hence it kills both cancer cells and normal dividing cells. Consequently, patient experience side effects such as
- Alopecia
- Appetite changes
- Constipation or diarrhoea
- Myelosuppression - Anaemia, neutropenia, thrombocytopenia,
- Nausea and vomiting - Acute, delayed, anticipatory
- Neuropathy
- Oral mucositis
- Skin photosensitivity
- Teratogenic and temporary or permanent sterility
Treatment Goals
To manage the expectations of the patients and their relatives, they should be well informed about the treatment goal.
Palliative chemotherapy
- Indicated for the most patients with widespread metastasis.
- To improve quality of life; survival increments are secondary.
Adjuvant chemotherapy
- To eradicate the micrometastatic disease that remains after an initial intervention that is designed to cytoreduce the tumour bulk.
- To achieve improvement in disease-free and overall survival.
Neoadjuvant chemotherapy
- Chemotherapy is administered before a planned cytoreductive therapy to
- result in a reduced requirement for surgery
- increase the likelihood of successful debulking
- reducing the duration of hospitalisation
- improve the fitness of the patient prior to interval debulking
Chemoprevention
- To prevent cancer developing in patients identified as being at particular risk.
Chemotherapy Administration
If we look at administration aspect of the chemotherapy regimen, it is not that straightforward. To illustrate, in FEC, we should administer epirubicin first before fluorouracil and cyclophosphamide.
As the rule of thumb, any drug known to be a vesicant should be given first when multiple drugs are prescribed (but certainly after any premedication). It is at this time, the integrity of the vein is the greatest and extravasation is the least likely. For practical reasons, drugs to be given by infusion, for example dacarbazine, should be administered last.
Common vesicants should include
- Anthracyclines (e.g. daunorubicin, doxorubicin, epirubicin, idarubicin)
- Vinca alkaloids (e.g. vinblastine, vincristine, vindesine, vinorelbine)
- Dactinomycin
- Mitomycin
# For the complete list of vesicants and irritants, you may refer to Ministry of Health Systemic Therapy Protocol page 131 or Management of Chemotherapy Extravasation: ESMO Clinical Practice Guidelines, 2012.
If doxorubicin and paclitaxel must be used concomitantly, to administer doxorubicin prior to paclitaxel and diligently monitor for the development of doxorubicin toxicity (e.g. congestive heart failure).
- Paclitaxel administration has been shown to decrease the clearance of doxorubicin (and doxorubicinol) to a clinically significant extent, resulting in increased toxicity (e.g. congestive heart failure). The mechanism of this interaction is unclear, but may be related to competition of metabolite isoenzymes (e.g. CYP3A4) or transport protein (e.g. p-glycoprotein).
- Docetaxel does not appear to share this same interaction potential, and thus may be a better therapy choice in some clinical situations.
When administered as sequential infusions, taxanes (paclitaxel, docetaxel) should be administered before platinum (cisplatin, carboplatin) to limit myelosuppression and enhance efficacy.
Only methotrexate, cytarabine and thiotepa can be given by the intrathecal route.
- Diluents used for intrathecal drugs should be preservative free.
- Inadvertent intrathecal administration of other cytotoxics, in particular parenteral vinca alkaloids, has caused death.
Carboplatin Calvert Formula
Most of the chemotherapy drugs that you see in oncology settings are based on body surface area. Carboplatin is a drug that you uniquely find that there is a special formula. Initially, carboplatin dosing is also based on the body surface area, but it resulted in a variable degree of thrombocytopenia, with a number of patients requiring platelet transfusion. Hence, Calvert formula becomes the adopted standard.
Dose = AUC target * (GFR + 25)
Few important key points that I would like to highlight here.
- The dose calculated in here is already the total dose in mg to be given to the patient. There is NO further need to multiply it with body surface area.
- Typical target AUCs lies between 4 and 7, depending on the frequency of administration, previous treatment and the drugs being used in combination.
- Currently, in Malaysia, the estimated GFR is still most commonly based on Cockcroft-Gault equation. In oversea settings, the Jelliffe formula is also commonly used. Both methods can underestimate or overestimate the GFR.
- A 2017 study suggested that BSA-adjusted CKD-EPI is the most accurate published model to predict GFR.
- An older study (2012) determined that the MDRD and CKD-EPI equations performed poorly compared with the reference standard radionuclide GFR; the Cockcroft-Gault equation showed smaller bias and higher accuracy in their oncology population.
- Capping estimated GFR at a maximum of 125ml/min is recommended by FDA to avoid potential toxicities.
- For patients with a GFR or CrCl less than 15 to 20ml/min, the use of Calvert formula is not recommended based on insufficient accuracy.
- In obese patients, some clinicians prefer to use an adjusted body weight; the adjustment factor may vary based on practitioner and/or institutional preference.
NOTE: Carboplatin is more stable in dextrose 5% than normal saline (sodium chloride 0.9%). What is actually happening? Due to the presence of chloride ions in normal saline, carboplatin could be converted to cisplatin.
Relevant links:
- Appropriate chemotherapy dosing for obese adult patients with cancer: American Society of Clinical Oncology clinical practice guideline
- GlobalRPh Carboplatin AUC Calculator
- GlobalRPh Carboplatin AUC Calculator (Updated Version-2017)
- New Model for Estimating Glomerular Filtration Rate in Patients With Cancer
Drug Associated Side Effects
Alkylating agents or procarbazine - Carry the risk of causing permanent male sterility
Anthracyclines (e.g. doxorubicin, epirubicin, idarubicin) - Cardiotoxicity and also causes urine discolouration (red).
Bleomycin - Pulmonary toxicity occurs in approximately 10% of patients; initial symptoms include cough and sometimes fever.
Cisplatin - Nephrotoxicity and ototoxicity (may consider carboplatin as alternative)
Cyclophosphamide and ifosfamide - Risk of haemorrhagic cystitis
Irinotecan - Acute and delayed diarrhea
Methotrexate - Mucositis, hepatotoxicity
Vinca alkaloids - Peripheral neuropathy (associated less with vindesine)
NOTE: Premedication with corticosteroids is recommended for taxanes (e.g. docetaxel and paclitaxel) to reduce the incidence and severity of fluid retention (docetaxel) and severity of hypersensitivity reactions (docetaxel and paclitaxel).


good sharing!
ReplyDelete