Focus in Outpatient Pharmacy
Introduction
The healthcare system in Malaysia has led to overcrowding of the pharmacy department in government facilities, even during the COVID period.
- Due to the COVID pandemic, lots of patients' appointments with doctors was extended with few months' prescription without a proper medical review by doctors.
- Nonetheless, outpatient pharmacists are still working tirelessly as usual to serve patients, despite being mentally exhausted due to the workload.
30-Minute Waiting Time
The key performance indicator previously used at outpatient pharmacy setting was to achieve a waiting time of 30 minutes from the time of receiving prescription to dispensing the medications.
- This shows how ambitious pharmacist staffs are to achieve a high efficiency with an error-free work.
Various factors contribute to length of waiting time, making this target unrealistic in certain settings.
- The need of transcribing in PhIS (for pharmacy-based facilities)
- The type of medications (if include extemporaneously prepared syrup or psychotropic drugs),
- Number of medications on a prescription slip,
- Number of patients already on waiting list and
- Number of staffs on duty (new or experienced, any staffs away from work due to emergency leaves, meetings or holiday)
- Any needs to do intervention(s) on a prescription slip
NOTE: In reality, these factors are never universally consistent across settings.
To many of us, outpatient pharmacy is a war zone.
- With a 30-minute target, everything is being rushed, starting from screening, transcribing, filling to dispensing. Sitting at outpatient counter, we are stressed by the stacks of medication baskets next to us.
- When dispensing error occurs and worst if it harms the patient, we are the one to be blamed too. We could not excuse ourselves with high workload, lack of manpower, exhausted mind or carelessness.
While to achieve a minimum waiting time is important, it should not be only focus. Quality care, including thorough medication checking and good medication counselling, is more important.
- In other words, Quantity should not be our only focus, but quality.
- Also, maybe it is time for us to review waiting time to 1 or 2 hours depending on facility workloads.
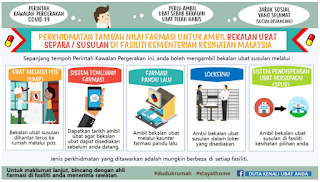
Value-Added Services
At Malaysia, medications are literally FREE to all Malaysians if they are having their clinical follow up at government facilities. To ease the process of patients obtaining their medication supply and reduce patients' waiting time, pharmacists have come up with numerous innovative ideas, such as
- Sistem Pendispensan Ubat Bersepadu (SPUB)
- Sistem Temujanji
- Ubat Melalui Pos 1Malaysia (UMP1M)
- Farmasi Pandu Lalu atau Kaunter Park & Take
- Locker4U
- MyUBAT
- Ubat Susulan Melalui Pihak Ketiga (UM3)
NOTE: Depending facility settings, there could be slight variation in local policy.
However, providing these value-added services is very labour intensive and time consuming.
- To illustrate, when providing Sistem Pendispensan Ubat Bersepadu (SPUB), manpower is required to request order, to prepare order and also to receive order.
- Documentations are also required in processing all the value-added services.
Nonetheless, some patients still dissatisfied with the services when their demands are not met.
- Often, the request is against the existing standard operating protocol or Poisons Act 1951.
- Plus, there are many patients who did not attend on the appointment dates given (e.g. for SPUB, Temujanji, Farmasi Pandu Lalu, Locker4U), which not only means our efforts are wasted but we also have to unpack and return the prepared medications.
As a matter of fact, pharmacists do not study 4 years to learn to pack medications for patients and our professionalism should not be valued by quantity of value-added services offered.
- In other words, pharmacist primary purpose is NOT to act as a medicine vending machine.
On the other hand, we should recognise that there are lots limitations associated with these value added services with the sole aim to provide convenience to patients.
- The patient consultation step (i.e. the key role of a pharmacist) is skipped.
- Hence, patients may not be well informed on brand changes or they are not able to ask for further clarification on the drugs.
- Proper storage and handling of medications during postage is in doubt.
- Fridge items (e.g. insulins) and nitroglycerin tablet should not be supplied by postage.
- There is NO quality assurance study that proves the medications are properly stored when handled by pos laju service (i.e. below 30°C). In fact, some heat sensitive medication tablets actually melted.
- If patient has been taking a drug wrongly due to unawareness of the change, medication errors cannot be detected early.
- When patient is readmitted to wards and have medication change or passed away, the medication that is posted to patient's home contributes to medication wastage and unnecessary workload.
- Patient do not have a proper channel to inform pharmacist that they have excess medication (e.g. not taking pain killers or other prn medications, receiving same medications from multiple health care facilities, receiving medications from ward admission).
- Lots of manpower is required to provide these value-added services, hence indirectly worsens the counter waiting time.
Patient Care Process
The core task of an outpatient pharmacist remains to fulfil patient medication-related needs through a patient care process. I have seen numerous circumstances of
- Patients having two prescriptions of different statins or proton pump inhibitors from different clinics.
- Patients are taking same medication of two different brands because they do not know it is the same drug.
- Patients only aware of the dose changes when they are collecting medications at pharmacy counters.
- Patients is facing adverse effects (such as cough due to ACE inhibitors or gastric irritation due to metformin) and asking for pharmacists opinion.
- Patient is allergic to paracetamol but doctor still prescribing paracetamol on the prescription.
- Patient is recently pregnant and has been on perindopril, but she has not gone for obstetric check-up.
- Unintentional omission of medications by prescriber
It is at these circumstances where you can see the true value of a pharmacist.
- Pharmacists are not your Shopee or Lazada, who supply your medication based on the request in a prescription.
- At the background, pharmacists are doing active checking on indication and dosage of medications for each prescription.
Medication Counselling
Medication counselling involves receiving professional advice from a pharmacist about new medication or devices, such as administration method and potential adverse effects.
During one encounter at the dispensing counter, a patient reported taking nystatin syrup for oral candidiasis, but had not seen much improvement.
- After some questioning, the patient revealed that he has been swallowing it directly like other antibiotic syrup.
- I then explained to him that he should swish the liquid around the mouth for as long as comfortable before swallowing.
Sometimes, pharmacists are not teaching sophisticated things to a patient, but just tiny little reminders.
Almost on a daily basis, we saw prescriptions of GTN tablet. Whenever patients ask a new supply of the sublingual tablet, I like to ask them, how long does it last once opened.
- Surprisingly, some of them will start guessing, is it 2 weeks, 1 months or 2 months.
- Many patients have never use GTN tablet for years after their first episode and may benefit from re-counselling.
NOTE: In-person (physical) counselling is more approachable than virtual counselling, which may be limited by slow internet connections.
Medication Therapy Adherence Clinic
Medication Therapy Adherence Clinic or MTAC is an ambulatory care service provided by trained pharmacists to improve patient understanding and adherence to medication.
However, recruiting long-term, well-educated patients with no compliance issue for these clinics offers little to no value.
- To maximize the potential benefits with limited staffs, a more targeted approach is necessary, such as selectively recruiting MTAC patients and enforcing structured and practical discharge criteria.
Comments
Post a Comment