Clinical Pharmacy
Introduction
Clinical pharmacy encourages pharmacists and pharmacy support staff to shift their focus from product orientation to more direct engagement with patients, to maximise the benefits that individuals obtain from the medicines they take.
History
The emergence of clinical pharmacy as a form of professional practice has been attributed to the poor medicines control systems that existed in hospitals during the early 1960. Although provoked by similar hospital-associated problems, the nature of the professional response differed between the USA and the UK.
- In the USA, the approach was to adopt unit dose dispensing and pursue decentralisation of pharmacy.
- In the UK, the unification of the prescription and the administration meant this document need to remain on the hospital ward and required the pharmacist to visit the ward to order medicines.
Clinical pharmacy developed from the presence of pharmacists in these patient areas and their interest in promoting safer medicines use. This was initially termed "ward pharmacy", but participation in medical ward rounds in the late 1970s signalled the transition to clinical pharmacy.
- Initially, the progress in professionalism in hospital pharmacy was gauged in terms of minimizing errors in dispensing and administration of medicines, and it has evolved to also focus on improving prescribing and ensuring that the intended results from medication use are achieved.
In other words, medication safety may have been the spur, but clinical pharmacy in the 1980s grew because of its ability to promote the cost-effective use of medicines in hospitals.
Clinical Pharmacist Roles
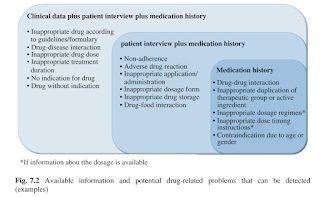
Pharmaceutical care is the term most often used to describe what a clinical pharmacist does. It entails regular monitoring of drug treatment for each patient under their care, including screening prescription charts for safety, appropriateness, efficacy and side-effects.
In fact, a wide variety of activities is associated with clinical pharmacy practice, such as
- Clinical research, including clinical trials (phase II or III)
- Drug therapy counselling, including bedside dispensing
- Drug information services
- Drug protocol management, such as renal dosing and drug interactions
- Drug therapy monitoring, including laboratory data and pharmacokinetic consultation
- Drug-use evaluation for hospital formulary
- In-service education
- Medication history taking and medication reconciliation
- Participation in medical rounds
- Total parenteral nutrition participation
Routine Jobs
How can a clinical pharmacist contribute to patient care process?
Obtain medication history using CP1 within 24-48 hours of admission.
- Identify if there is any known food or drug allergy.
- Assessing patient adherence and understanding on their drugs.
- Perform medication reconciliation for newly admitted or transferred-in patients to ensure all patient's medications are correctly endorsed on the medication chart to ensure continuation of care.
Reviewing patient medical note and drug chart
- Perform a quick medication management review and identify any possible intervention.
- Justify the prescribing of the drugs in patient clinical context.
- Initial and date all drugs on a drug chart to imply that a "clinical check" is made, including drugs that is rewritten from previous chart.
- Indication, dosing, frequency and duration.
- Endorse drugs with their non-proprietary approved names, unless they are combination products with no approved names.
- Brand names can be added for medication where the brands are not interchangeable, such as Prograf and Advagraf.
- May make a remark on drug chart if the drug endorsed is a closed formulary medication (e.g. started by consultant XX).
- Dosing time and prandial advice should be specified on the drug chart as appropriate, including dosing date for methotrexate and alendronate.
- May make a remark on dilution and infusion rates for unusual medications, such as oral vancomycin.
- Drugs stored in the refrigerator should be endorsed "Fridge".
- Any special dosing of drugs may also be supported with reasons written on drug charts so that pharmacists at inpatient can take note.
- Identify and monitor patients who require therapeutic drug monitoring and parenteral nutrition and other drugs which require close monitoring.
- May make a remark on sampling time on drug chart for TDM purpose.
Participate in ward round
- Answer queries from doctors, such as drug availability or drug dosing.
- It is fine to take some time to find out the answer, but always remember to feedback the findings.
- Provide recommendations on medical therapy.
- Selection of a drug choice should be made after considering patient clinical conditions (such as renal function, liver function, G6PD deficiency, blood count and pregnancy), concurrent medications (verify if there is any drug-drug interaction that requires dosage adjustment or change in drug therapy) as well as the potential benefits and risks of different medications.
Patient counselling
- Improve patient's knowledge and understanding on drug therapy, including device techniques such as insulin or inhalers.
- May suggest patients to purchase Aerochamber if needed.
- Counsel patients on common adverse effects of medications and issue allergy card when identified.
Bedside dispensing
- Ensure all medications are endorsed completely and correctly on the discharge prescription.
- Identify if there is any medication change by comparing to CP1 form earlier.
- Counsel patients on medication changes and newly started drugs.
It may seem easy to perform all these tasks for 1 patient, but when a clinical pharmacist has to repeat it for 15-20 patients daily, the workload becomes enormous. Probably, to accomplish all at the start is nearly a mission impossible because some hiccups is always there.
CP Forms at Malaysia
At Malaysia government hospitals, there are 4 important CP forms that we use in clinical pharmacy.
- CP1 Medication History Assessment Form
- CP2 Pharmacotherapy Review
- CP3 Clinical Pharmacy Report Form
- CP4 Patient Referral Note
NOTE: These CP forms may also be used at other pharmacy settings too.
Summary
Clinical pharmacy is not just about being on the wards.
- It is about the thought process behind what you are doing.
- It is about using your knowledge and expertise to improve patient care.
Comments
Post a Comment